Colonial administrations introduced various social infrastructure in Africa. Scholars have studied their effects on education (Brown, 2000), and health care (Lasker, 1977; Patterson, 1981; Huillery, 2009; Lowes & Montero, 2021). A recent paper (Vrooman, 2023), compares the development of colonial health care provision in Ghana and Côte d’Ivoire. In this study, colonial health care provision is defined as all factors of production that are employed in providing health care goods and services by the colonial administration. For example, it includes labour, capital, and clean water used in colonial health care services that were administered by colonial rulers. The paper also studies the development of colonial health care provision and colonial health care policies within these countries over time. To this end, it analyses four aspects of colonial health care provision in Ghana and Côte d’Ivoire using new data constructed from colonial reports: finance, health care facilities, medical staff and patients.
Colonial expenditures on health care provision
For the majority of the first half of the 20th century, deflated colonial health care expenditures (in per capita terms) were higher in Ghana than in Côte d’Ivoire (Figure 1). As for the percentage of colonial health care expenditure of total expenditures by the British and French colonial administrations, a similar, although less pronounced, difference between Ghana and Côte d’Ivoire is found. Subcategories of each budget are considered to dissect these colonial finances further. The medical branch (tasked with medical care) was initially prioritized in the British colonial medical budget but after the First World War, the sanitary branch (responsible for hygiene and preventative measures) started to catch up. The French colonial administration divided their medical expenditures between expenditures on staff and material, of which the former received the largest share (especially until the number of health care facilities started to increase after the initial decades of the 20th century).
Figure 1: Deflated annual expenditures on medical services per capita in Ghana (GHA) and Côte d’Ivoire (CIV), in francs, 1897-1955
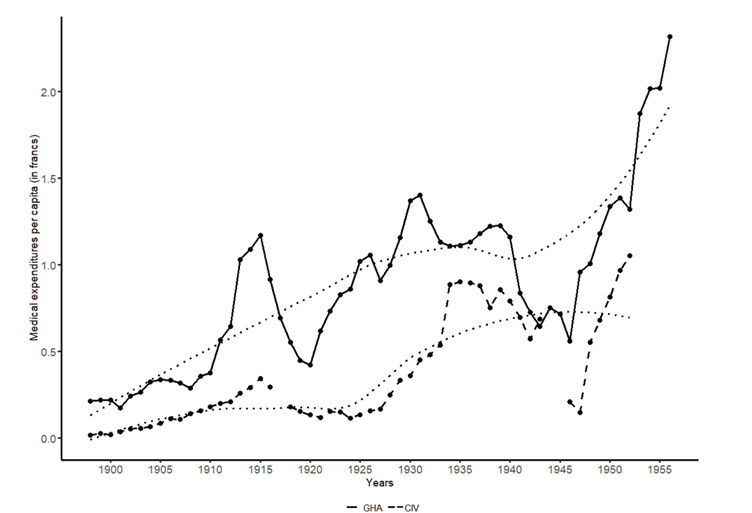
Source: Vrooman (2023, p. 225) based on data from colonial reports.
Colonial health care facilities
As for the expansion of colonial health care facilities, a difference between Ghana and Côte d’Ivoire is found throughout the first half of the twentieth century. Initially, the number of facilities was low in both countries, but the geographical coverage differed. In Ghana, facilities were located in the south in areas with a sizeable European population, whereas in Côte d’Ivoire health care facilities were more spread out as French colonial administrators also considered the administrative and economic importance of locations around this time. By the 1930s, the networks in both countries had widened considerably (Figure 2), following changes in British and French colonial policymakers’ views on social policies. In Ghana, the expanded network of health care facilities reached nearly all regions of the colony and consisted primarily of colonial hospitals and dispensaries (Figure 2). A similar widening of the network occurred in Côte d’Ivoire, as all districts were incorporated in the health care structure by the 1930s. The medical posts managed by the Assistence Médicale Indigène (AMI, indigenous medical assistance) were the most prominent. By the end of colonial rule, the expansion of colonial health care facilities continued in Côte d’Ivoire while in Ghana the number of health care facilities decreased following the abolition of segregated facilities in 1944.
Figure 2: Colonial health care facilities in Ghana (GHA) and Côte d’Ivoire (CIV) in 1931
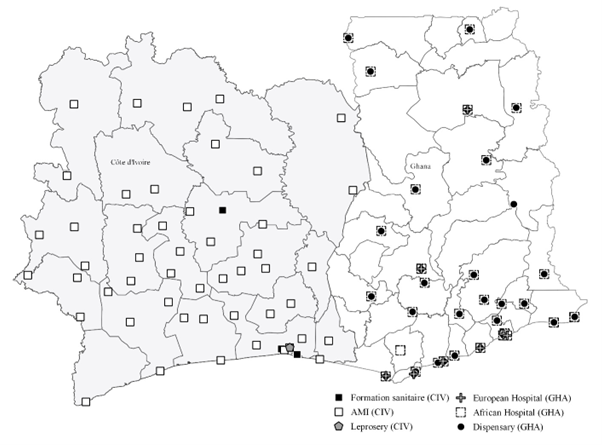
Source: Vrooman (2023, p. 231) based on data from colonial reports.
Colonial medical staff and patients
The findings on medical staff show a reversal in the patterns: a larger number of staff (per capita) were initially employed in Ghana compared to Côte d’Ivoire, but this was reversed by the 1920s. The division of labour also differed between the two countries. In Côte d’Ivoire, nurses formed a substantial part of the colonial staff base over time, while a larger variety of staff functions were employed in Ghana. For Côte d’Ivoire, the increases in the number of colonial medical staff (per capita) as of the 1920s-1930s are shown to have been driven by the employment of additional Ivorian staff members (Figure 3).
Figure 3: Colonial medical staff by origin (per 100,000 people) in Côte d’Ivoire: 1897-1942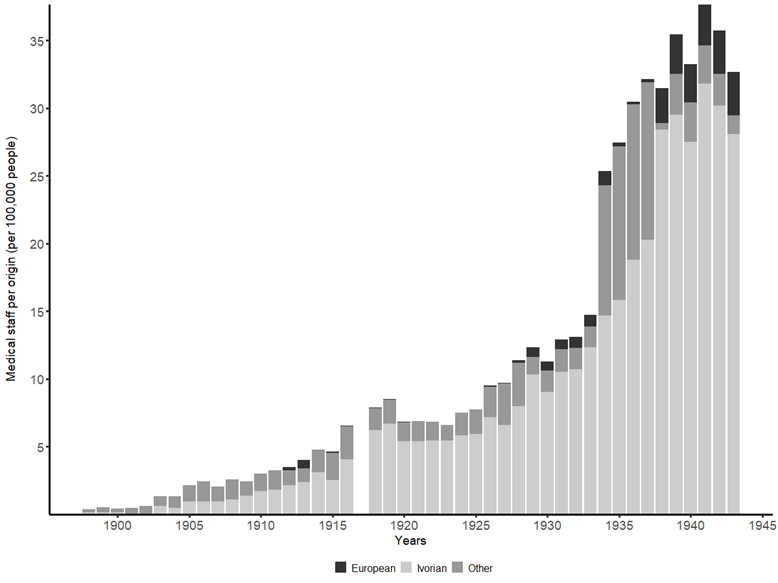
Source: Vrooman (2023, p. 240) based on data from colonial reports.
Finally, the number of patients treated within colonial health care facilities in both countries is considered. The number of patients (per capita) began to increase substantially in Ghana only once the British policy stance had widened toward social development by the late 1920s. Further increases occurred in the decades afterward, with outpatients rising substantially during the 1940s. The trend in Côte d’Ivoire is similar.
Health care provisions as a factor for social development
This study highlights the need to consider colonial health care provisions as an integral part of evaluating colonial legacies on social development in Africa. Even two neighboring countries with similar conditions such as Ghana and Côte d’Ivoire are shown to have different health care trajectories, resulting in different starting points for their post-independence health developments. At present, we continue to observe health inequalities across the African continent (see e.g. WHO, 2018, p. 14), and history may help us to better understand the roots of these inequalities.
References
Brown, David S. 2000. “Democracy, Colonization, and Human Capital in Sub-Saharan Africa.” Studies in Comparative International Development 35 (1): 20-40.
Huillery, Elise. 2009. “History Matters: The Long-Term Impact of Colonial Public Investments in French West Africa.” American Economics Journal: Applied Economics 1 (2): 176-215.
Lasker, Judith N. 1977. “The Role of Health Services in Colonial Rule: The Case of the Ivory Coast.” Culture, Medicine and Psychiatry 1: 277–297.
Lowes, Sara, and Eduardo Montero. 2021. “The Legacy of Colonial Medicine in Central Africa.” American Economic Review 111 (4): 1284–1314.
Patterson, K. David. 1981. Health in Colonial Ghana: Disease, Medicine and Socio-Economic Change, 1900-1955. Waltham, MA: Crossroads Press.
World Health Organization. The state of health in the WHO African Region: An analysis of the status of health, health services and health systems in the context of the Sustainable Development Goals. Brazzaville: WHO Regional Office for Africa, 2018. Retrieved from https://apps.who.int/iris/handle/10665/275292
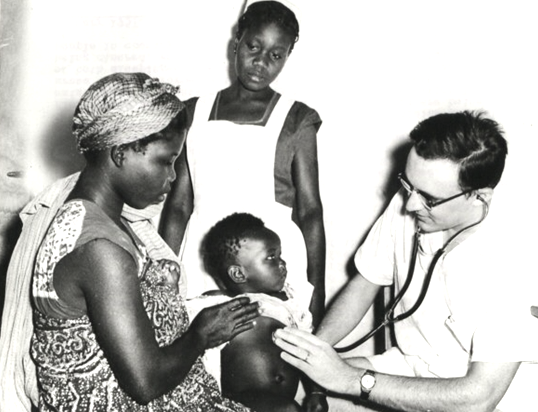
Feature image: A British doctor examines an African baby at a maternity and child welfare clinic. Source: The National Archives. CO 1069-46-7